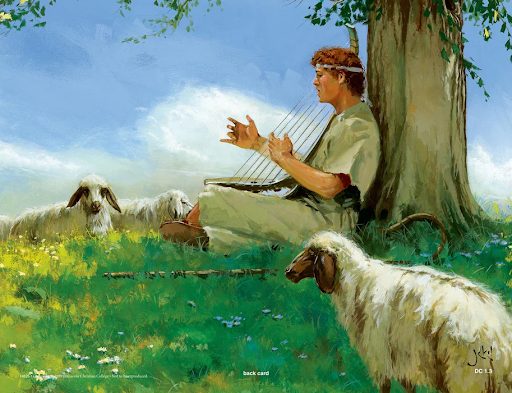
“Whenever the spirit from God came on Saul, David would take up his lyre and play. Then relief would come to Saul; and he would feel better, and the evil spirit would leave him.” 1 Samuel 16: 23
“Now there were four men with leprosy at the entrance of the city gate. They said to each other, ‘Why stay here until we die? If we say, ‘We’ll go into the city’– the famine is there and we will die. And if we stay here we will die. So let’s go over to the camp of the Arameans and surrender. If they spare us, we live; if they kill us we die.’ At dusk they got up and went to the camp of the Arameans. When they reached the edge of the camp, no one was there, for the Lord had caused the Arameans to hear the sound of chariots and horses and a great army, so that they said to one another, ‘Look the king of Israel has hired the Hittite and Egyptian kings to attack us!’ So they got up and fled in the dusk and abandoned their tents and their horses and their donkeys. They left the camp and ran for their lives. The men of who had leprosy reached the edge of the camp, entered one of the tents and ate and drank. Then they took silver, gold, and clothes, and went off and hid them. They returned and entered another tent and took some things and hid them also. Then they said to each other, ‘What we’re doing is not right. This is a day of good news and we are keeping it all to ourselves. If we wait until daylight, punishment will overtake us. Let’s go at once and report this to the royal palace.’” 2 Kings 7:1-9
I share these scriptures with a dose of irony to make the claim that our healthcare systems are in dire straits. There is a disease eating away at the vitality of it’s functioning, so as a society we are at a crossroads where we must make a decision based on what we know. One of the biggest problems of our generation are the barriers to access to quality care and treatment adherence, which create disparities in health outcomes globally. A key explanation for this trend is the systematic negligence of culture as a determining factor of whether or not individuals will be receptive to national and local health guidelines. Today, increasing awareness is being brought to the connection between the mind and body. With this increased consciousness it has become apparent that it is no longer acceptable to compartamentalize the individual into four distinct parts, but rather the four aspects of a person’s existence (i.e. the physical, social, emotional, and spirital/existential according to the WHO) are always intermingling with the other. A person is an ecosystem in itself, if one aspect is altered, it will have cascading effects on the other. This realization poses the question whether it is ethical to see several specialists to address health disruptions for each of the four domains or rather one that can prescribe fewer, more encompassing treatment options. Consider Post-traumatic Stress Disorder, a multifacted condition that is categorized primarily as a psychological issue, but often has great consequences on physical, social, and existential well-being:
Physical:
- Stunted growth
- Asthma
- Increased reactivity of the amygdala
- Reduction in the size of the hippocampus and prefrontal cortext
- Reduced serotonin concentration
- Drastic changes in weight
- Sleep deprivation
- Consistently low cortisol levels and elevated corticotropin-releasing factor (CRF)
- High blood pressure and heart rate
Social:
- Isolation
- Suspension or routine leaves from school or work
- Aversion to people, places, or situations that elicit flashbacks
- Characterized as defiant or volatile by peers, loved ones, etc.
Spiritual/ Existential:
- Inability to see a future for themselves – higher risk for suicide, self-harm and/or self-medicating
This is not an exhaustive list, but researcher and psychiatrist Dr. Bessel van der Kolk, talks extensively about the failures to properly assess PTSD patients in his recent work Body Keeps the Score. He discusses how it is more typical for those with PTSD to be diagnosed with several different psychological and/or physical conditions such as, Attention Deficit Hyperactivity Disorder, anxiety disorders (like Obsessive Compulsive Disorder, Generalized Anxiety Disorder), mood disorders (e.g. Bipolars Disorder and Major Depressive Disorder), obesity, and eating disorders. As a result, they are often prescribed several different kinds of medications (sometimes to balance the effects of other medications), or have need to see several different specialists, to address symptoms that are associated with every condition, but the root. Our patients’ bodies are not test tubes. In these cases, having an intimiate relationship between patient, physician, and family members is crucial to being able to come to a proper diagnosis, and thus, the best treatment plan for the individual. Although drug treatments have seen great progress, their prescription is not always aligned with the values of the patient, nor do they make sense in the context of the indivdual’s age, comorbidities, or financial status. Shall we not live on more than pills alone? The good news is that as new findings and insights on illness and quality of life are brought to the fore through narrative medicine and narrative-based research methods, innovative and holistic cures are being considered to address the complex intersectionality of health. The development of programs promoting the use of art therapies and cures, are the fruit of these endeavors. Surely if we were to do nothing with this new information, and not undetake further investigation to verify its potential we would be doing the world a great disservice. So please be proactive with this news, carefully read and take to heart the proposed solutions to the major issues our society is being plagued with that are written in this book. Take this chance and live.
